Cayman first jurisdiction in region to boast variant detecting equipment, vital to green-listing
Cayman’s ability to conduct genome sequencing is not only a pivotal leap forward for the local COVID response, but it could also help give the jurisdiction the edge it needs to be added to the UK’s ‘green’ travel list.
Health Services Authority CEO Lizzette Yearwood made this point when she discussed the new technology on the Cayman Crosstalk radio show on 8 June.
“Once we can identify what is happening here in this community, we upload it into a global database. [W]e have had a lot of discussion with the Governor’s Office about this, because this technology and the information we get from these tests is really going to help us in our negotiations with the UK to get us in the green status, so we are very excited about the work,” Yearwood said.

HSA molecular biologist Jonathan Smellie has been conducting the genomic sequencing at the lab. – Photo: Alvaro Serey
At present, Cayman is on the UK’s amber list, which requires that travellers from here must quarantine for 10 days upon arrival in Britain. HSA recently announced the Cayman Islands Forensic Science Laboratory has commenced this specialised testing, the first to be done regionally outside of the Caribbean Public Health Agency (CARPHA).
Chief Medical Officer Dr. John Lee praised the advancement, noting: “[G]enomic sequencing… will have applications in the identification of a number of different infectious diseases, in the management of other medical conditions, and in other forensic work.
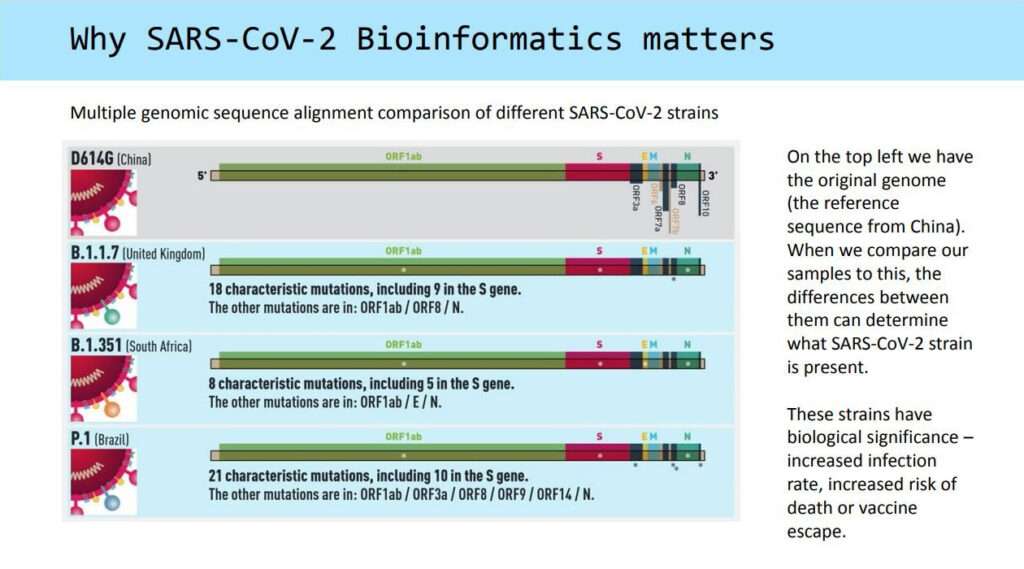
“In infectious diseases, genomic sequencing essentially gives us the ‘signature’ of each strain so we can track which one is causing an outbreak. It is a very technical process requiring a high degree of skill,” Lee told the Cayman Compass in an email.
Key tool in COVID fight
HSA molecular biologist Jonathan Smellie, who has been conducting the sequencing, said that having this technology on-island is a “big deal”.
“It’s important in many different ways. The immediate need for it is sequencing of SARS-CoV-2, and that is done all around the world. It’s been happening over the last year and so that’s really what we’re getting started with first,” Smellie told the Compass.
However, he said, there is much more scope with the technology they are now using at the laboratory.
HSA received two next-generation sequencing machines through donations from the R3 Cayman Foundation, the Caring for Life Foundation and an anonymous private donor.
Bryan Hunter, R3 Foundation chairman, said delivering on such a donation was more than worth it, given the benefits to the island, especially as it helps to determine the origin of variants.
“[It] helps us to contact trace the cases of COVID that we’re experiencing in Cayman and that all helps the jurisdiction to respond to viruses like the one we’re facing, and we understand that other jurisdictions which have this type of equipment have been able to use it to great effect when it comes to containing outbreaks,” he said.
Hunter added that having the equipment would help Cayman “prepare for, detect, [and] respond to variants [and] other viruses in a very effective manner, [mitigating] the risks for the jurisdiction when it comes to these types of pandemics going forward”.
How it works
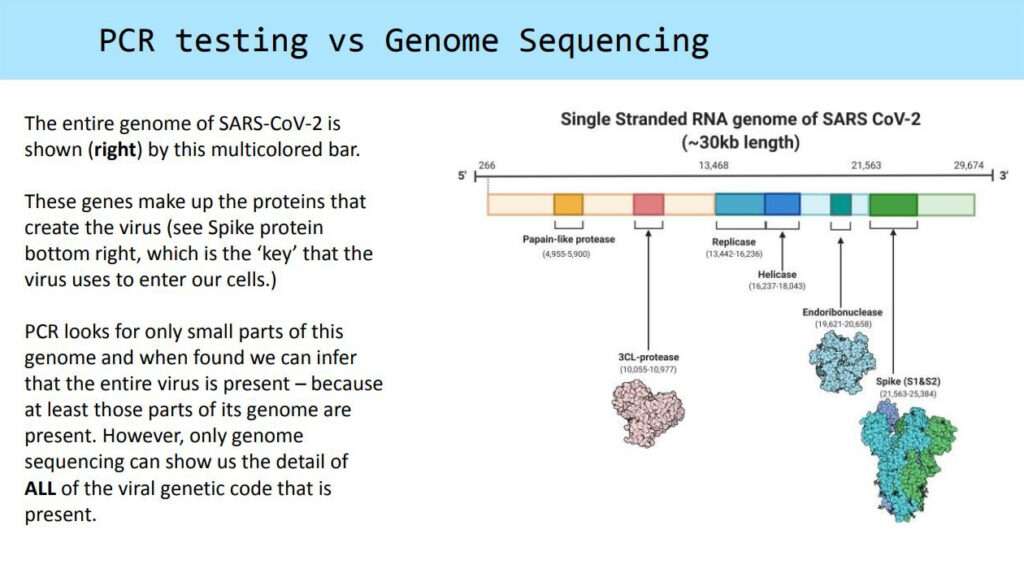
Prior to the use of genome sequencing, Cayman’s SARS CoV-2 capability only related to PCR testing, which detects the presence of the coronavirus from a patient sample – because at least those parts of its genome are present.
However, only genome sequencing can show the detail of every part of the viral genetic code that is in a sample.

This is one of the two genome sequencing equipment at the HSA that was purchased through donations from the R3 Foundation. Photo: Alvaro Serey
Smellie said the genome sequencing starts with the same nasal swab used for PCR testing. After the patient is swabbed, the sample then goes into a viral transport media or a solution.
“If there’s virus present on that swab, it gets suspended in that media and then it goes through to our lab and we process it. We inactivate the virus. If it’s present, then we extract and purify that genetic code leaving behind all the other material [such as mucus] that’s in that swab,” he explained.
It is run through a PCR test to determine whether there is actually virus in that swab.
“Once we’ve done that, we’ve detected the virus, then we can say it’s ready for sequencing because there’s no point in sequencing nothing. We can only sequence positive samples,” Smellie added, saying there is a special criterion for determining what type of positive sample to sequence, based on the amount of starting material “because this technique has its limits”.
“It needs a certain input of genetic material otherwise it can’t tell you everything. And so once we’ve determined that, we then start that [sequencing] process, and that is quite a long and complex process that involves a series of PCR reactions, and series of different reagents,” he said.
The sequencing sample is then prepared and gets loaded onto the sequencer instrument itself to determine what DNA/RNA letter is in each position of the genome.
At the moment, Smellie said, this process can take anywhere from 12 hours to days. “Once that’s done, then there’s a computer process that analyses the sequencing data to put it all together to eventually tell the strain of the virus present in the sample,” he said.
The sequencer instrument, the MinIon flow cell, can run up to 96 samples at one time and can be reused at least twice.
Increased testing capacity, new career paths Smellie said while the sequencing is now being used for COVID-19 variants, it will also be extended to screening for different types of cancers “that are most prevalent in the region and on-island”.
Added to that, he said, HSA is going to expand those sequencing services to do medical genetics, newborn screening, and genetics for certain types of inborn errors of metabolism (in which the body cannot properly turn food into energy).
All of these tests, he said, fall under the umbrella of precision medicine. Such testing can save lives, Smellie said, pointing to the example of checking newborns for diseases that may affect how they process nutrients.
“As a result of that difference in processing, that child’s health may be in danger if they’re not treated immediately. Being able to screen for those diseases that can cause that problem allows us to get ahead of that and treat them before there’s any damage caused,” he said.
Smellie said as a young Caymanian he was proud to have this technology here and to be a part of expanding the capabilities on-island, which in turn open up new career opportunities for locals.
He said at the moment HSA is training people in the data analysis software to be able to make sense of the information processed through genome sequencing.